This time of year in the midwest can be challenging. We have had perhaps a busy holiday season with back-to-back events, while balancing work and family responsibilities. Most days are cloudy, cold and dark.
But what happens to our brains this time of year that can trigger seasonal affective disorder – (SAD) or the winter blues? Digging deeper into this topic, it is critical to know that there is a difference between SAD and the winter blues, as outlined below.
What are the risk factors and causes?
There are several risk factors and causes that can contribute to someone developing SAD or winter blues. This includes family genetics, location of where you live, history of having a mood disorder, and having a low level of vitamin D. Let’s drill into these areas.
Family Genetics
When your therapist is getting to know you, the question of genetics is usually a topic of discussion. We know that genetics are a determinant for mental health diagnoses – including depression and anxiety. SAD is a form of depression that spikes during a particular season. If your family members are prone to low mood, then you are also at greater risk for having the same.
Asking family members about their experiences with mood shifts is important. Furthermore, understanding what medications people in your family are taking helps you to know what could work for you too. Psychotropic medications affect everyone differently, but if you know someone in your nuclear family takes one particular medication and it works, then it is more likely that it will work for you too.
Location of Where You Live
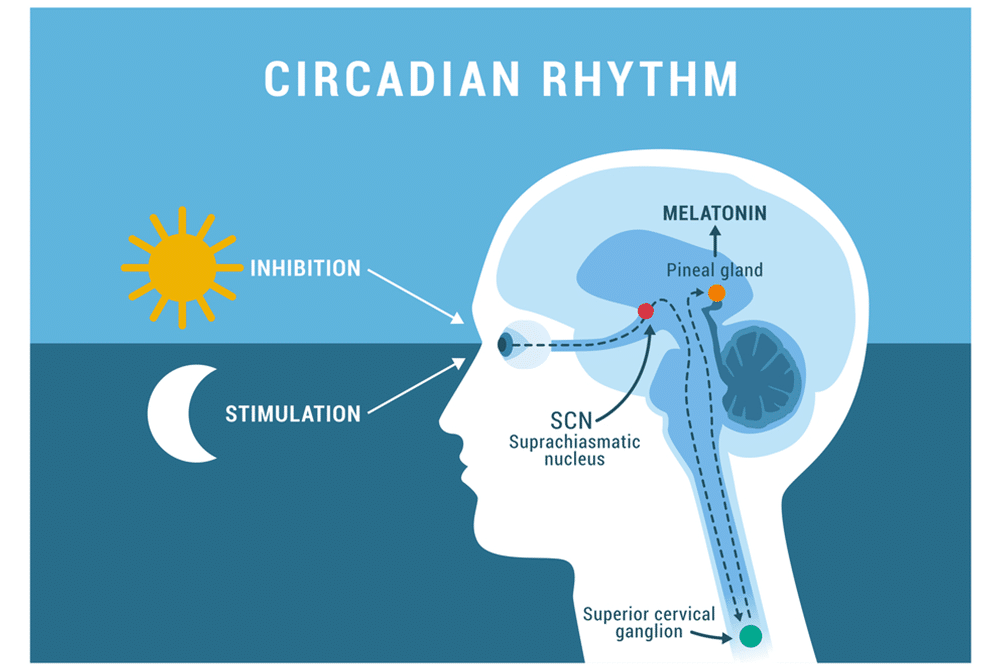
We sometimes take sunlight for granted, but definitely notice when it’s gone for extended amounts of time. We found an article by Julie Corliss from Harvard Health Publishing that discusses this. Corliss explains that “according to research, the reduction in daylight affects our circadian rhythm, which in turn has a domino effect. Not only does our circadian rhythm help with setting our internal clock for sleep and awake time, but it helps regular appetite and hormones (melatonin and serotonin most notably here) in our bodies.” Phototherapy (light therapy) can be a helpful tool if this speaks to you as a trigger. The light therapy can help stimulate your pre-frontal cortex which will in-turn help with emotion regulation.
History of Having a Mood Disorder
It could be that you are already diagnosed with depression or another mood disorder. Perhaps you’re noticing that your symptoms intensify during a particular season. This could be the case and if so, reaching out to your therapist and medication provider can help drive the discussion of treatment options. Maybe increasing your medication for this particular season and then decreasing again is an option that will work best for you.
Vitamin D
No doubt being in the midwest, with less sunlight, will affect vitamin D levels. Vitamin D is an essential nutrient that we can get from food sources and the sun. Speaking with your primary care doctor about a vitamin D supplement can be a way to supplement yourself for the low-light months ahead. A routine blood panel can help determine where your vitamin D levels are as well.
Winter Blues vs Seasonal Affective Disorder
Some questions to ask yourself include (but not limited to) – am I missing important life events/responsibilities, am I taking care of myself the way I would like to or typically do, are people in my life concerned about me, and am I having thoughts of not wanting to be alive. If you answered yes to any of these questions then perhaps this is more than winter blues and please reach out to a safe person immediately.
What Would Your Therapist Say?
Some ways to combat the winter blues or SAD…
- Routines of sleep, socializing, movement,and eating are key!
- Getting outside everyday – even if it is cold outside. Cold weather actually is grounding and helps regulate emotions – try it next time you’re triggered!
- Scheduling special events – date nights, movies, new experiences (cooking classes, painting, museums etc.)
- Regularly therapy and medication use – make sure you are scheduling at least bi-weekly this time of year for check ins
- Brighten up your environment – open the blinds/shades to encourage what natural light we can savor or consider your bulbs in your light fixtures
- Reduce or eliminate substance use – alcohol and other substances actually can cause us to just feel plain worse!
Please note that these are general guidelines from our experienced therapists and not to be substituted for medical advice from your general practitioner. If you have further questions please reach out to Leigh Rzepecki, LCSW, CADC.
Resources
- Vitamin D
- Mayo Clinic – Seasonal Affective Disorder
- Seasonal Affective Disorder: More Than a Feeeling by: Joel Streed
- Phototherapy/Light Therapy
- How to select a light box
- Harvard Health Publishing: Light Tjhrapy: Not Just for Seasonal Depression By: Julie Coreless
- CDC – Circadian Rhythm
- Dietary Guidelines for Americans – Food Sources with Vitamin D
Feeling like you’d like to explore this more? Contact Leigh Rzepecki, LCSW, CADC.